July 19, 2016 | News | New Publication
Why men feel healthier and women live longer
In most countries, men score pretty well in assessing their own health and physical functioning. Yet they have a lower life expectancy. The paradox is especially pronounced in Russia, where men on average die eleven years earlier – yet they are healthier. Or are they not?
(The following text is based on the original article Sex Differences in Biological Markers of Health in the Study of Stress, Aging and Health in Russia by researchers Anna Oksuzyan, Vladimir Shkolnikov and James W. Vaupel from the MPIDR, Maria Shkolnikova from the Scientific Institute of Pediatry at the Pirogov Moscow Medical University, and Kaare Christensen from the University of Southern Denmark and has with minor changes also been published in the issue 2/2016 of the demographic quarterly Demografische Forschung Aus Erster Hand.)
To look into this question, Anna Oksuzyan and colleagues from the Max Planck Institute for Demographic Research in Rostock analyzed data on the health of Muscovite men and women. The data came from the study "Stress, Aging, and Health in Russia" (SAHR), as part of which more than 1000 men and women aged 55 and over provided information on their health. Among other things, on a six-figure scale they evaluated their own health and provided information on their physical functioning, such as the extent to which they are limited in performing activities that vary in challenge, for instance, bathing, getting dressed or running. At first, the results painted a familiar picture: The women did less well than the men in subjective health and in evaluating their physical functioning. But can women really be unhealthier despite having a higher life expectancy? Or are they just more ready to moan?
To learn more about male and female health, the SAHR involved conducting interviews as well as measuring, weighing, and scanning: Diverse biomarkers, i.e., measurable parameters on metabolism, cardiovascular activity, blood lipids, or inflammation markers were derived from the study subjects; valuable data that allowed the researchers to look under the skin of the respondents.
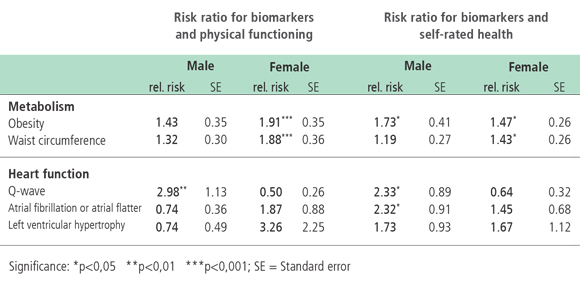
Tab.1: Women who are obese often have significantly lower physical functioning whereas men with certain ECG abnormalities (abnormal Q-waves) often report poor or very poor self-rated health. © Source: SAHR, own calculations
And they saw that men are not necessarily healthier than women; they simply have different strength and weaknesses in health. To put it casually, women are suffering more from waist-related health problems and men more from heart-related problems (cf. Table 1). There was no clear tendency in the level of blood pressure and blood lipids and no sex differences at all in inflammation markers. But the scientists found specific gender differences in body weight and body size on the one hand and heart disease on the other.
For instance, some 60% of the women have too large a waist circumference, whereas this is true for only about one in three men. Obesity is much more widespread among female Muscovites too than it is among the city’s male inhabitants. Abnormalities of the heart such as atrial fibrillation and hypertrophy, by contrast, are much more common among the men than they are among the women. To find out whether the biomarker values are related to the health information verbally reported by the study subjects, the scientists divided them each into two groups. Those with poor self-rated health (“poor”' or “very poor”) and with physical functioning in the lowest quintile were collapsed into one group; those with relatively better subjective health were combined into the other group. The division showed a clear link between the biomarker values and the subjective health of the study subjects. The obese women, for instance, have a risk almost twice as high to belong to the group with poor physical functioning than the women of normal body weight. Among the men, the association between electrocardiographic abnormality, in the so-called Q-wave (which may indicate, for instance, a heart-attack at some time in the past) and physical functioning is especially high. Men with an abnormal Q-wave have a risk three-fold higher to be significantly limited in physical functioning than other men.
Here the female and male authors of the study see a possible explanation for the gender differences in self-rated health: Excess weight, though not directly life-threatening, may nevertheless lead to many health disadvantages and years of suffering. Men, by contrast, may feel fit and healthy for many years and then die of a sudden heart attack. In this sense then, the paradox in Russia may be explained at least in part: Men feel healthier, but they are not necessarily so.
More Information
Anna Oksuzyan, Maria Shkolnikova, James W. Vaupel, Kaare Christensen, Vladimir M. Shkolnikov, Sex Differences in Biological Markers of Health in the Study of Stress, Aging and Health in Russia, PLOS ONE, June 5, 2015