April 27, 2021 | Press Release
Varying COVID-19 Case Fatality Rates

Why did COVID-19 claim seven times more lives of those infected in Italy compared to South Korea? © iStockphoto.com/vlada_maestro
In Italy, around one in seven people suffering from COVID-19 died at the end of June 2020 compared to a good two percent of those infected in South Korea. These differences are largely explained by the age structure of people who had tested positive for COVID-19, but to some degree they also reflect differences in the extent to which the healthcare systems were overburdened.
(The following text is based on the original paper Monitoring trends and differences in COVID-19 case-fatality rates using decomposition methods: contributions of age structure and age-specific fatality by MPIDR researcher Alyson van Raalte. A German version with minor changes has also been published in the issue 01/2021 of the demographic quarterly Demografische Forschung Aus Erster Hand.)
A simple formula can be used to calculate how deadly the SARS-CoV-2 virus is: the number of people who died from the virus divided by the number of people infected.
For South Korea, this yields a figure of 0.022 for the end of June 2020, meaning that 2.2 percent of those confirmed as infected died from the virus, whereas in Germany lethality was more than twice as high, at 4.6 percent. And in Spain and Italy, as many as 12 and 14 percent of those infected died in the summer of 2020, respectively, as shown by a study of Alyson van Raalte, Christian Dudel, Tim Riffe, Enrique Acosta, and Mikko Myrskylä of the Max Planck Institute for Demographic Research; and Cosmo Strozza of the Sapienza University of Rome.
To identify the likely causes behind these enormous differences, they analyze data from South Korea, China, Germany, the USA, Spain, Italy, and the City of New York. South Korea is the reference country because case detection was high due to extensive testing and because the pandemic had set in comparatively early.
Lethality from COVID-19 is largely determined by the age of those infected. The researchers thus establish two key components for their analysis: They compare the age structure of people afflicted in the individual countries and analyze the level of age-specific fatality rates, for example the percentage of infected 80-year-olds in Italy and in Germany who died.
Averaged over all countries, the age structure of the afflicted explains about two-thirds of the differences in case fatality rates, the result of their analysis shows. This can mean that simply a higher share of older people contracted the virus, thus they had a higher risk of dying.
Particularly at the onset of the pandemic, this might have been true for countries such as Spain or Italy, where contact between the generations is often more intense than, for example, in Central or Northern Europe. Later into the pandemic, COVID-19 outbreaks in nursing homes in particular could have caused infections to climb in older age groups.
However, higher incidence among older people is often a statistical phenomenon: For example, when tests are scarce, many asymptomatic and comparatively harmless disease trajectories are not tested and thus not included in the statistical calculations. Older people are more likely to be symptomatic, and thus have their infections detected.
A further analysis shows: In some countries, the age structure is not the main driver behind higher case fatality rates than those in South Korea. In the USA, and especially in New York City, the difference to South Korea is explained primarily by higher age-specific fatality rates as such: 56 percent in the United States and 77 percent (over two-thirds of the difference) in New York City.
To give an example: In South Korea, two percent of those infected aged 80-89 died compared to 4.2 percent in New York City (a percentage more than twice as high) during the period studied.
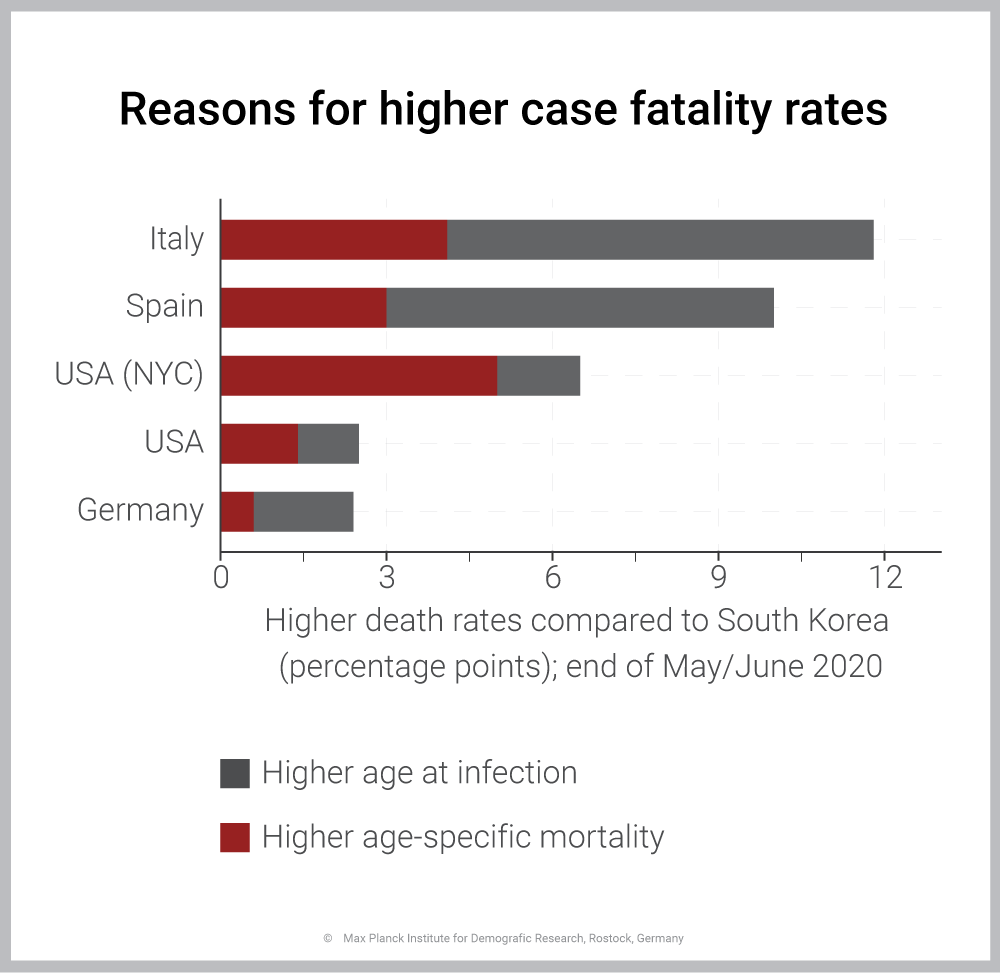
In most countries, case fatality from COVID-19 is higher because those infected were older compared to South Korea. In New York City, by contrast, higher age-specific fatality rates were key. Source: Statistisches Bundesamt, Statistische Landesämter, BBSR
Download Figure (PNG File, 41 kB)
According to the researchers, differences such as these probably stem from healthcare systems that are overburdened, running out of intensive care beds or ventilators for example.
But the number and kind of pre-existing medical conditions in people of this age group can also play a role. When a country has a large share of overweight people, for example, it can be assumed that age-specific fatality rates will be higher too.
Further analysis of the researchers also points to a healthcare system overwhelmed, an analysis for which they looked at infection numbers and at deaths in Italy during a period of about four months: In early March, a good four percent of those infected died compared to twice as many two weeks later. And by the end of May the proportion gradually rose to 14 percent.
A higher age-specific fatality rate among the infected bears the lion's share of this 90 percent increase (since early March). Here, too, it can thus be assumed that a healthcare-system overload caused the death toll to soar.
Time lags in reporting figures can cause distortions, too. For example, if a wave of infection is contained, infection numbers nosedive in some measure but many people still die of previous infections. Thus, a serious analysis of the numbers can usually be done only when the pandemic has subsided, the authors of the study write.
Current data should therefore be interpreted with caution. For example, the case fatality rate in Germany presently is around 2.7 percent, with 85 percent of the post-June 2020 reduction due to a younger age structure among those who tested positive and 15 percent the result of falling age-specific fatality rates. Here, too, it is not yet possible to gauge conclusively the extent to which these figures are distorted by time delays, Alyson van Raalte cautions.
She and her colleague stress that more antibody studies are needed to obtain a more solid database. Such studies would also look at random blood samples of people not infected but tested for antibodies to the SARS-CoV-2 virus to detect infections that may have gone unnoticed.
This would help to determine how many people truly contracted the SARS-CoV-2 virus. A detailed breakdown by age of those afflicted and those who died is essential for further analysis, too, the authors say.
Original Publication
Dudel, C., T. Riffe, E. Acosta, A. van Raalte, C. Strozza and M. Myrskylä: Monitoring trends and differences in COVID-19 case-fatality rates using decomposition methods: contributions of age structure and age-specific fatality. PLoS ONE 15(2020)9, e0238904. DOI: 10.1371/journal.pone.0238904